OVERVIEWNuclear medicine uses radioactive materials to diagnose and treat various medical conditions, such as thyroid gland cancers, lymphomas, hematomas, and other tumours. It helps specialists understand the functioning of organs, the growth of cancer cells, and tissue structure, providing information for treatment decisions. This speciality has been an integral part of medical care since the 1950s and has seen significant advancements in the last two decades due to progress in science and technology.
How Does Nuclear Medicine Work?
Nuclear medicine is a cutting-edge medical technique used in several medical specialities, including heart, gastrointestinal, neurological, and endocrinal conditions, and cancers. Radiotracers are injected into the body to project images with a detailed view, aiding in the assessment, evaluation, diagnosis, and treatment of various medical conditions.
Nuclear medicine therapy is another significant branch that employs radioactive iodine (I-131) for treating thyroid cancer, radioactive antibodies to combat lymphoma and metastases of tumours into the bones, and to stop the progression of cancer cells in adrenal glands in adults and tumours of nerve tissues in children. Radioimmunotherapy and brachytherapy are two other treatments under nuclear medicine that are yielding promising results in treating various types of cancers.
Applications
Nuclear medicine’s application lies in both the diagnosis and treatment of cancers.
Diagnosis of Cancer:
Nuclear medicine is an advanced radiology technique that helps diagnose cancer and tumour growth. Radiotracers, injected or ingested, accumulate in the body and give off gamma rays to detect areas of intense activity. Hot spots may indicate a tumour, while cold spots could also be indicative of tumour growth with less cellular activity.
1. PET/CT:
PET/CT is a powerful diagnostic tool, and during this procedure, a radioactive tracer is injected intravenously to detect cancers. It can also use contrast material to produce multiple 3D images. PET/CT is recommended for detecting cancer cells, tracking their spread to other organs, monitoring treatment progress, evaluating tissue viability, and detecting cancer recurrence.
Treatment for Cancer:
Nuclear medicine is used to treat a broad spectrum of cancers, and the following are the different nuclear medicine treatment options available:

Radioactive Iodine Therapy:
Radioactive iodine (I-131) therapy is a primary treatment for thyroid cancer that targets cancer cells and prevents them from spreading to other parts of the body. It is also used to treat hyperthyroidism.

Radioimmunotherapy:
Radioimmunotherapy, a combination of radiation therapy and immunotherapy, may be used to treat non-Hodgkin’s lymphoma patients who don't respond to chemotherapy. Monoclonal antibodies are injected into the body to target cancer cells and activate the immune system. It is also being studied as a potential treatment for other cancers, such as prostate cancer, colorectal cancer, leukaemia, melanoma, and brain glioma.
Brachytherapy:
Brachytherapy is a non-invasive or minimally invasive cancer therapy wherein a radiation source is placed close to or inside the tumour. This procedure delivers high doses of targeted radiation to specific areas, killing cancer cells with fewer side effects. It is effective in treating cancers of the breast, brain, cervix, endometrium, esophagus, bile duct, and head and neck.
Nuclear Medicine at HCG
HCG is committed to providing advanced diagnostic and treatment options to its patients. The fully-fledged nuclear medicine department at HCG features state-of-the-art diagnostic and therapeutic platforms for managing a broad spectrum of cancers.
The following are the features of the nuclear medicine department at HCG:
- Two advanced SPECT CT Gamma Cameras are available in our department.
- We have two top-of-the-line digital PET CT machines, the Siemens Vision 600, to provide high-quality diagnostic support.
- The department boasts ten dedicated isotope therapy rooms, making it the largest theranostics facility in India.
- Our nuclear medicine experts have extensive experience administering I-131 therapies for thyroid cancer and targeted isotope therapies, such as Lu177 PSMA and Lu177 dotatate.
- Our nuclear medicine department, in collaboration with the interventional radiology department, is the first in the country to offer intra-arterial therapies using Lu177 Dotatate, Actinium Dotatate, Actinium FAPi, Actinium Dotatate therapies, and I131 Lipiodol for hepatocellular cancers/hepatic metastases.
Firsts from HCG’s Nuclear Medicine Department
- First centre in India to establish a medical cyclotron to produce PET CT tracers as per CGMP norms. It is the only centre to produce 10 different types of PET tracers on a routine basis to solve complex clinical diagnostic challenges.
- First hospital in India to offer Actinium (Alfa) therapies for advanced cancers of the prostate and neuroendocrine tumours.
- India’s first hospital to offer FAPi scans on a daily basis.
- India’s first centre to offer Lu177/Actinium FAPi therapies for FAP-positive advanced cancers.
- India’s first centre to obtain NABH MIS accreditation for imaging services using the PET CT platform.
Theranostics
HCG is committed to providing top-notch cancer care and constantly strives for innovation in diagnostics and treatments. One of the significant achievements of our nuclear medicine department is the introduction of theranostics in cancer care for the first time in India. The term “theranostics” is derived from the phrases, “therapeutics” and “diagnostics.” Theranostics is the integration of diagnostics and therapeutics to concurrently or sequentially diagnose and treat medical disorders, which is a game-changer for modern medicine. HCG's patient-centric approach aims to save time and money and prevent negative outcomes, making theranostics a perfect fit for our cancer care model.
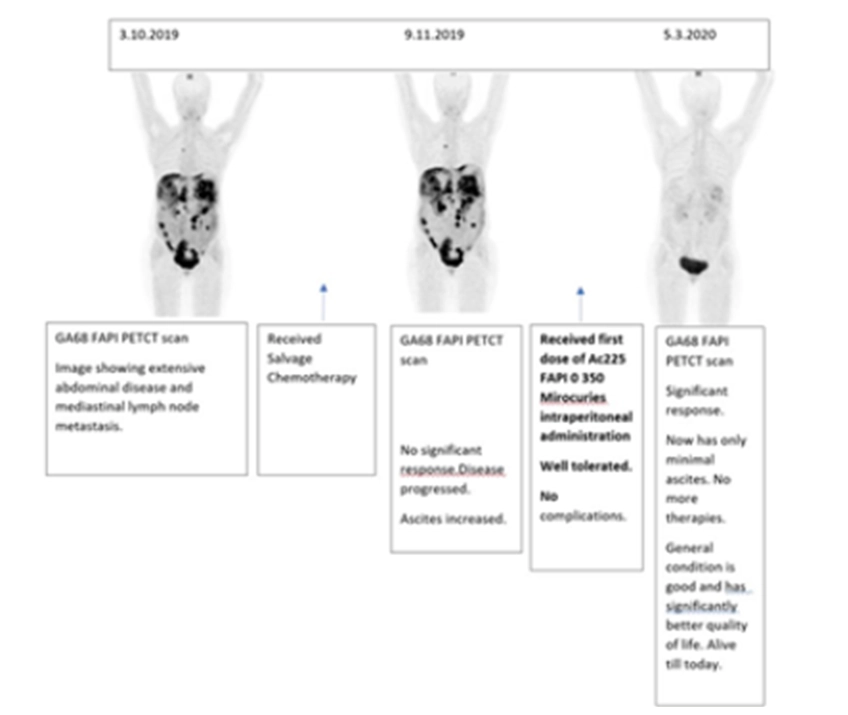
Case Study Demonstrating the Efficacy of Theranostics:
A 50-year-old woman presented herself with carcinoma of the ovary. She had undergone all established therapies for her condition. However, her body showed no response, and the disease started progressing. As a last resort, a Ga68 FAPi scan was performed, which revealed an advanced disease. This was followed by Ac225 FAPi therapy, and the patient showed excellent treatment response. Currently, many end-stage cancers are being treated similarly, especially when there are no other promising treatment options.